need to be aware of the most common and lesser-known manifestations of the disease. This presentation intends to introduce clinicians to the complexity of PD symptoms and prepare them for timely diagnosis and appropriate management. Specifically, it will describe the impact of Parkinson’s disease on the brain, dopamine, and substantia nigra’s role in its development, most common signs and symptoms, and several lesser-known manifestations.



Signs and symptoms of PD(Parkinson’s Disease)
tremor Bradykinesia Rigidity Postural instability Micrographia Speech changes Masked face Non-motor symptoms; Cognition sleep Mood. This presentation also includes diagnosis, treatment, and further management when a multidisciplinary approach is needed. It describes how to live with a condition and what caregivers should take into account.
Table of Contents
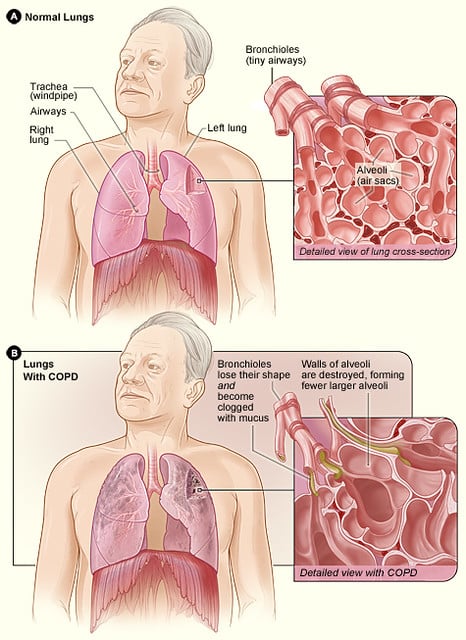
Parkinson’s disease usually develops when certain nerve cells in the brain, primarily those responsible for producing a chemical called dopamine, become impaired or die. Dopamine is a neurotransmitter that sends signals to the part of the brain that controls the many movements made throughout the day. When dopamine levels decrease, the symptoms of Parkinson’s disease manifest, becoming increasingly severe as time passes. Parkinson’s disease is the second most prevalent neurodegenerative illness worldwide, surpassed only by Alzheimer’s disease, and impacts millions of humans . Although it is more common in the elderly, it can also affect younger individuals, albeit rarely. For the reasons mentioned, it is critical to pay close attention to the symptoms of Parkinson’s disease and quickly recognize them. Early treatment might help regulate the disease’s symptoms more effectively, leading to improved patient quality of life. In addition to that, the earlier the disease is detected, the sooner treatment may begin to establish therapies that aim to slow progression and maintain motor functions. Finally, increasing knowledge among the general public about the symptoms of Parkinson’s disease could result in a quicker diagnosis and access to healthcare. This article examines the symptoms of Parkinson’s disease further, with a focus on both motor and non-motor features to improve comprehension and detection and optimize treatment. Parkinson’s Disease Understanding Parkinson’s Disease: Parkinson’s disease is a multifaceted neurodegenerative disorder that harms the brain’s ability to manage motion. Furthermore, it is a condition marked by the gradual decimation of certain neurons in the brain, predominantly those lying in the substantia nigra, the region that creates dopamine. What is Parkinson’s Disease? Parkinson’s is a movement ailment, but its effects on motor function are not all. Instead, it is caused by neurons malfunctioning and dying, especially dopaminergic neurons. Dopamine is a neurotransmitter that aids in the regulation of motion.
Parkinson’s Disease Causes
2.How Parkinson’s Disease affects the brainLoss of dopaminergic neurons in the substantia nigra, a small brain nucleus deep within the brain, is one of the hallmarks of Parkinson’s disease . These specific neurons are essential for conveying the help of many signals responsible for controlling movement and coordination. When dopaminergic neurons degenerate, the brain has a reduced amount of dopamine. The lower the dopamine level, the more substantial the dysfunction in the delicate neurotransmitter balance and the more visible the motor symptoms of PD. 3. . Role of dopamine and the substantia nigra in PD. Dopamine serves as a neurotransmitter that conducts signals between brain neurons. It is essential in coordinating smooth, controlled movement between muscle pairs. When the disease gradually kills these neurons, it cripples the production and release of dopamine, resulting in the described movement problems .
Second, the substantia nigra AP LD surround the basal ganglia, a group of nuclei in the brain related to movement, forming an important connection to it. Dopaminergic basal ganglia muscular involvement that provides disturbances within the generation and execution of voluntary movement. The diminished levels of dopamine levels allow the basal ganglia to control the muscles unequally. It gives rise to the motor signs of apathy that distinguishes tremors, slow movement, rigid muscles, and imbalance – reducing postural tremor sway. Understanding the roles of dopamine in the substantia nigra and the basal ganglia is crucial for learning about Parkinson’s disease and finding ways to restore coordinated dopamine action through an adequate aimed at improving motor function. 3. Common signs and symptoms. Parkinson’s disease has shown several symptoms that might impact a person’s life daily.
These include:
Tremors.The most classic and well-described symptom of PD is tremors, which affect approximately 70-80% of patients. Parkinsonian tremors present at rest, typically starting on one hand or arm and then affecting other limbs and, in advanced cases, the face. Tremors related to PD are rhythmic and involuntary, and they often take the form of a pill-rolling tremor or repetitive movement resembling the rolling of a pill between the thumb and fingers . Although this tremor is most severe during periods of relaxation and inactivity, the patient may experience relief from tremors when engaging in or executing purposeful, goal-oriented movements or sleep.
Bradykinesia–
Bradykinesia, or slowness of movement, is the other cardinal symptom of PD. Patients with PD may have difficulty starting and executing voluntary movements. Patients often appear sluggish or reluctant to initiate actions. Essential everyday activities such as walking, ascending and descending a chair, or performing fine-motor tasks like buttoning a shirt may become considerably slower and more challenging. This symptom may severely hinder daily functioning and freedom, limiting their ability to bathe, feed, and dress independently and preventing them from leading a normal life.
Muscle rigidity—
Muscle rigidity, or stiffness, is a prevalent symptom amongst PD patients. It is assumed to result from increased resistance to passive movement or muscle tone, resulting in a tight feeling in the affect áreas d muscles. dequeueReusableCellWithIdentifierentially experience pain and discomfort. The most frequently affected areas are limbs but also the neck and trunk.
Postural Instability:
Postural instability refers to the impaired balance and coordination that characterizes Parkinson’s disease, putting affected individuals at risk of falls and fall-related injuries. People with PD may have difficulty maintaining an upright posture and may assume a stooped or forward-leaning posture. In addition, they may have a propensity for swaying or loss of balance, lack of equilibrium, especially when attempting to turn or change direction . Postural instability results from the combination of muscle rigidity, bradykinesia, and impaired proprioception, which is the body’s ability to discern its orientation in space. Thus, postural instability needs to be addressed to avoid falling and boost patients’ overall mobility and independence. It is critical to familiarize oneself with these and other major Parkinson’s disease symptoms to facilitate early diagnosis, accurate assessment, and on-time intervention for improved disease management and overall quality of life of affected persons.
* Lesser-Known Signs and Symptoms In addition to tremors, bradykinesia, muscle stiffness, and postural instability, which are more common symptoms of Parkinson’s disease , the following lesser-known problems also impact patients’ daily life and functioning:
1. Micrographia:
Micrographia is a peculiar alteration in one’s writing style. Specifically, individuals with Parkinson’s disease experience micrographia, characterized by small, cramped, and illegible handwriting that progressively worsens over time .
Asik Akhan:
This problem is thought to be caused by PD-induced bradykinesia or voluntary fine motor control difficulties. Micrographia may make writing tasks challenging for patients, influencing their social interactions through writing notes, signing documents, or filling out forms.
Changes in speech are another fairly common non-tremor symptom of PD. Speech can be characterized by different nuances, such as a decrease or increase in utterance loudness or inarticulate pronunciation. Also, the voice of the patient himself may be blurred, muffled . Hypophonia is the term that describes a quiet, low tone of speech with little variation in loudness and pitch . When people speak, the words may merge, leaving a rather monotonous line. This feature of speech is due to a disruption in the signals to the muscles responsible for the voice. People around may not understand everything that a patient can say. Naturally, this causes the development of depressive conditions and strong psychological discomfort;
Masked face.
The facial expression of a patient with PD may become less mobile and expressive . In other words, we can observe a kind of ”mask’; on the face, that is, it is difficult to understand whether the person is happy, angry, or sad. As a result, facial paralysis can lead to a decrease in emotional expressions, which ultimately causes misunderstandings and discomfort in communication with patients. In terms of the causes, the ability to control facial muscles and activate them is lost due to the paralysis of the regulation center in the brain. Consequently, bradykinesia and impaired muscle motor functions contribute to such a symptom. It is essential to be aware of the above-listed signs to improve patient compliance and support patients properly. A more profound knowledge of the problem will have a positive effect on the work of medical workers and provide maximum care for PD patients throughout the course of the disease.
It is crucial to recognize less-known symptoms of Parkinson’s disease and integrate their management to provide more comprehensive care. Awareness of manifestations above is important for promoting PD patients’ ability to communicate effectively and maintain their social connections and overall well-being.
5. Non-Motor Symptoms Parkinson’s disease presents as a movement disorder, but it is also associated with a complex array of non-motor manifestations that significantly impact a patient’s overall health and quality of life. Key non-motor symptoms associated with PD are highlighted below:
Cognitive Changes Cognitive impairment, ranging from abnormalities in memory and attention to full-blown dementia, is an increasingly recognized feature of Parkinson’s disease.
Not all PD cases are associated with dementia, but cognitive changes occur in an extremely high percentage of cases, especially as the disease progresses. Typical symptoms include impairments in frankly attentional tasks, memory, executive function, and difficulty multitasking and planning.
In advanced cases, clinical symptoms can also include outright memory disorders and confusion. Parkinson’s disease dementia is the most severe form of cognitive impairment seen in PD, characterized by significant memory and executive function impairment, and an overall decline in ability. Sleep Disorders Finally, sleep disorders are extremely prevalent among PD cases and negatively impact patients’ quality of life . Common PD sleep problems include insomnia, where a patient finds it hard to either fall asleep or stay asleep, and restless leg syndrome. Restless leg syndrome is characterized by uncomfortable sensations that worsen at rest and get better with movement. Another characteristic problem seen in PD is REM-sleep behavior disorder . Patients with RBD act out vivid, often violent dreams during REM sleep, risking injury or awakening to the patient and their bed-sharing companion.
Mood Disorders
Asik Akhan:
The next cluster of non-motor symptoms that have a devastating impact on the quality of life for individuals living with PD is the mood disorders . Some of the most common mood disorders that affect PD patients include depression, anxiety, and apathy. Depression, for example, is the most common non-motor symptom of PD and affects up to 50% of patients at some point in their disease encounter. Depression refers to a feeling of sadness, loss of interest or pleasure in activities, hopelessness, or worthlessness, and changes in sleep or eating habits . Anxiety remains a significant mood disorder among PD patients and involves worry, fear, and nervousness. Apathy, a feeling of lack of motivation or interest in previously enjoyable activities, is also common . An independent factor that fuels emotional and social withdrawal is well-defined by mood disorders; thus, it is fundamental that thorough treatment management considers non-motor symptoms. It is crucial to identify and treat all non-motor symptoms in developing an appropriate management plan that maximizes patients’ well-being. Proper and effective interventions and management strategies enhance better results for patients and their caregivers.
Imaging Scans:
Parkinson’s disease has no specific test that can be used to conclude its diagnosis. However, imaging tests such as magnetic resonance imaging and dopamine transporter scan are useful. The two scans are used to support the diagnosis by uncovering the areas in the brain related to PD. These MRIs will show low dopamine levels and any structural changes in the brain.
Treatments:
Medications:
Parkinson’s disease is managed using medications that help the body to produce dopamine or serve as dopamine . Levodopa is a precursor to dopamine and is the most effective drug in treating motor symptoms of PD. Other drugs used include dopamine agonists, MAO-B inhibitors, and COMT inhibitors.
Therapies:
Physical, occupational, and speech therapies are useful in treating and management of Parkinson’s disease. These therapies help the people to modify the symptoms of PD and promote growth motor function, balance, and speech.
Surgery:
Surgery is also used to treat advanced PD. Deep brain stimulation is a surgical procedure used in treatment. It involves the implantation of electrodes in the brain to control abnormal neural activity and treat motor symptoms. Multidiscipline approach. PD is a multisystem disorder and, therefore, requires a multidisciplinary approach. Care by neurologists, movement disorder specialists, rehabilitation therapists, nurses, and social workers guarantee holistic care to suit the victims. The professionals will ensure a customized care plan, given the disease severity, individual choices, and quality of life.
When Parkinson’s disease is accurately diagnosed, targeted treatment interventions are offered, and coordinated care is provided, healthcare professionals can help patients and their families/loved ones lead fulfilling lives despite the challenges posed by the disease:
Living with Parkinson’s disease presents unique challenges, but there are many available strategies and support systems to help individuals manage their symptoms and maintain a good quality of life.
To control motor symptoms and promote better daily functioning, it is necessary to follow drug therapy regimens recommended by a specialist. It is equally important to communicate more openly with healthcare providers about treatment steps and side effects of specific medicines.
Healthy lifestyle —
Since symptoms management and improvement are related to regular physical activity, good nutrition the best diet is also helpful, and getting restful sleep proper, the patient can also increase resilience . Stress management Stress can also provoke motor symptoms, so relaxation techniques, mindful breathing, and other approaches may be helpful. . Supportive strategies for daily living .
Asik Akhan:
Boards, spoon sticks, speech therapy to correct sounds and syllables – the use of these techniques allows removing the daily difficulties Routine visits to the doctor upon examination, it is much easier for the specialist to predict the progression of the pathological process and to quickly help with the ascent of other symptoms, replacing the prescription Opinions on the beneficial effect of active physical exercises on the functional state are contradictory. Most experts agree that regular classes – at least three times a week – can help achieve several goals: .
Physical Therapy:
A physical therapist can develop a workout routine tailored to your unique needs, which may include gait training, balance exercises, and mobility-enhancing solutions. Physical therapy may also help alleviate pain, rigidity, and postural disorders which often accompany PD. Support Groups: Attending Parkinson’s disease support groups, whether in person or virtually, that provide emotional backup, practical advice, and a sense of community for people with PD and their caregivers. Working with people who have been through similar problems can make you feel powerful and relaxed while exchanging stories, coping strategies, and resources. Tips for Caregivers and Loved Ones:
Get Informed:
Educate yourself on as much PD as possible, including its symptoms, progression, care options, and ways to assist. Knowing more about it will allow you to give knowledgeable and loving care.
Focus On Open Communication: Keep the conversation flow open with the patient, the healthcare provider, and the rest of the care team. Promote honest discussions on symptoms. treatment preferences, and fears or worries.
Self-care: Caring for a loved one may be tough on the body and mind. Your well-being should take priority, so make sure to get some breaks, contact friends or family, and engage in hobbies.
Patience and Flexibility: Parkinson’s signs may fluctuate and duties may change. Techniques such as patience, versatility, and resourcefulness can shift to help address caregiving problems and adapt to various needs. By remembering these techniques and using the support systems that are appropriate for them, people with Parkinson’s illness may improve their lifestyle, freedom, and capability to participate in activities that are meaningful to them. Furthermore, recognised ones fulfil vital supportive roles by providing excellent care, education, and support to those living with PD during this journey.